InfoPFT is a software-based project for interpreting pulmonary function tests, based on cybernetic artificial intelligence tools. Built on the foundations of respiration pathophysiology, InfoPFT aims to evolve to a more integral analysis of the functional disorders of lung and respiratory system diseases (P.V. Romero Colomer “Guia de Interpretación de las Pruebas de Función Respiratoria”. Elsevier ed.. Barcelona, 1 vol 135 pp, 2021). InfoPFT application provides a tool to help physicians produce comprehensible pulmonary reports, taking into account the global functional status obtained by pulmonary function tests. From simple spirometry to complex functional studies, diagnosis is made by taking into account the ensemble of significant parameters and the coherence of redundancies.
The strength of the functional diagnosis is based on the reliability of the dysfunction pattern description which often depends on the selected set of tests. The following three properties are important for this purpose:
- Redundancy: Dispose of independent parameters carrying the same or similar information that are mutually reinforcing, especially when they are in the limit of the normality range (FVC, SVC, FRC, TLC in previously described pattern reinforce the diagnosis of restriction).
- Coherence: Parameters carrying complementary information pointing in a given direction (RV, RV/TLC, KCO are coherent with the diagnosis of alveolar occupation)
- Concordance: Degree of fitting or appropriateness of dysfunction pattern to clinical diagnostic and morphological findings according to our knowledge of clinical-functional and structure-function relationships.
It is important to take into account that the functional impact of changes in a given parameter can be amplified or weakened by the redundant and coherent effect on other aspects of lung function (a “mild spirometric” obstruction becomes functionally (and clinically) less “mild” if it induces a severe air trapping, hyperinflation or hypoxemia for instance). In contrast with some classical methods of functional diagnosis, the functional impact is less related to the individual deviation from “normal” values than to the combined effects of different functional troubles.
Pulmonary function tests
Pulmonary function tests explore different aspects of pulmonary (respiratory) function. Usually, several categories of parameters can be identified: those exploring ventilation, gas exchange, pulmonary circulation, oxygen transport or response to exercise. Obviously, all these parameters interact with one another in such a way that, for instance, ventilatory dysfunction nearly always influences gas exchange or response to exercise, and so on.
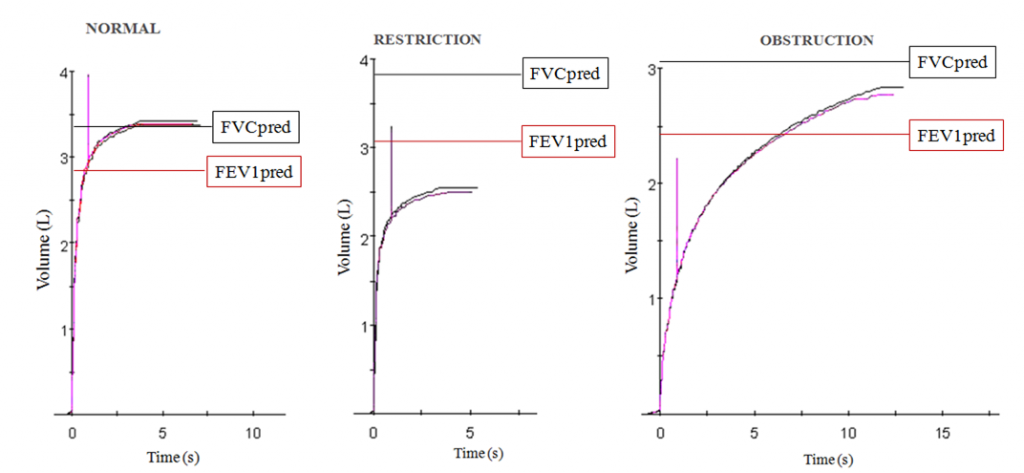
In clinical practice, functional diagnosis usually begins by identifying ventilatory dysfunction through forced spirometry. Forced spirometry is the simplest and most consolidated test of pulmonary function, and consequently, it is very useful for an initial approximation to the evaluation of the ventilatory status of the lung and respiratory system. Forced spirometry has three main parameters: Forced Vital Capacity (FVC), Forced Expiratory Volume in one second (FEV1) and the percent ratio between both (FEV1%FVC). FVC is the maximal volume that can be exhaled forcibly after a maximal deep inspiration; FEV1 is defined as the amount of gas that can be exhaled in one second after a maximal inspiration and during a maximal forced expiratory maneuver.
FEV1 is the parameter that best evaluates the global ventilatory disorder for several reasons:
- Because it decreases both in airways obstruction and in a ventilatory restrictive defect, (see Figure). When both situations are present (mixed syndrome) the effects are additive on FEV1..
- Because it is narrowly related to maximal ventilatory capacity (maximal ventilation that the subject can perform for 20 seconds, expressed in L/min)
- Because it is a well defined and well-used parameter, employed in large epidemiological studies, with good reproducibility.
- Because it can be measured with only one second of forced expiration after maximal inspiration, even if the subject stops the forced maneuver before reaching maximal expiration (sometimes the patient’s clinical status forces acceptance of minimal but useful information).
To be more precise in the diagnosis of ventilatory dysfunction we will need other explorations to provide information that composes the complete picture of the Functional Diagnosis of Ventilatory Dysfunction (see Table). Furthermore, we can analyze the interactions between ventilatory dysfunction and troubles of non-ventilatory parameters like pulmonary hemodynamic, gas exchange, oxygen transport to tissues, and exercise tolerance.
TABLE: Characteristics of Ventilatory Dysfunction
|
Vector |
Intensity |
Direction |
Primary Char. |
Secondary Char. |
Interactions |
|---|---|---|---|---|---|
| VENTILATORY DYSFUNCTION |
Mild Moderate Severe Very Severe |
Obstructive |
Upper AW Central AW |
Superior Extrathoracic Intrathoracic Turbulences Malacy |
Resp. Failure P. Hypertension Gas Exchange Exercise Limitation |
|
Bronchial Generalized Peripheral Bronchiolar |
Reversibility Maldistribution Collapsibility Compression alv.gas Gas Trapping Static hyperinflation Dynamic hyperinflation Hyperresponsiveness Airways Inflammation |
||||
|
Mixed |
Mix |
Mix |
|||
|
Restrictive |
Thoracic Disease Neuromuscular Pleuropulmonary Alv. Occupation Lung retraction |
↓Lung Expansion ↓Air/Tissue Ratio Heterogeneity Hypoventilation Pulmonary Retraction Bronchial Traction Intrinsic muscles dysf. Extrinsic muscles dysf. ↓Compliance RS ↓Total Lung Volume Congestive lung Hypoventilation |

Recent Comments